- Academia
- For Corporate
- Cashless Facilities
- Media
- Donate
#NoCompromise
- 020 6609 9888 | +91 9168013322
#NoCompromise

Our eyes are like a camera with a lens and a film at the back of the eye. The retina is the light-sensitive layer at the back. All images coming through the lens of the eye get focused on the retina. The retina converts these images into signals and sends them to the brain via the optic nerves.
Long-standing or uncontrolled diabetes can damage the retina causing diabetic retinopathy.
In the early stages, it has no symptoms and can be detected only through an eye examination. If detected early and treated, it is possible to control the disease and retain vision. Both medical, laser and surgical treatments provide relief. But if left untreated, it leads to irreversible vision loss, and ultimately permanent blindness.
High blood sugar levels harm all organs of the body, including the eye. Over time, high sugar can weaken and damage tiny blood vessels in the retina This can cause several complications including cataracts, glaucoma, diabetic macular oedema and diabetic retinopathy.

An estimated 11.4% of the Indian Population (101 million people) have diabetes, while as many as 15% (136 million people) are pre-diabetic.
Unfortunately, many people may be unaware of their sugar level, which is hence uncontrolled. We recommend that everyone should undergo basic health check up and blood tests, at least once in a year. Your doctor will prescribe the tests that are required.
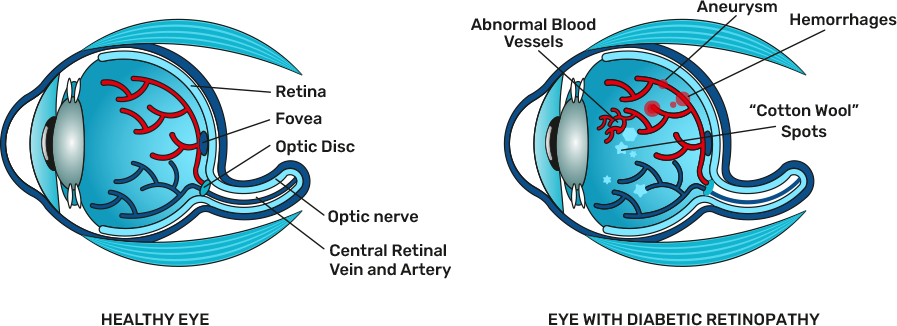
The retina is the delicate inner lining of the eye that sends visual messages to the brain via the optic nerves. When blood vessels in the eye are damaged, they cause blood or fluid to leak into the retina. When this happens, the retina swells up and your vision is affected.
As the disease progresses, scar tissue and abnormal blood vessels may develop which are very delicate. If these abnormal blood vessels burst, blood will fill the back of the eye and prevent light from reaching the retina. This will result in loss of vision.
You may have diabetic retinopathy,
either with, or without symptoms.
You may have diabetic retinopathy, either with,
or without symptoms.

(Regular clinical evaluation is required)

(With or without symptoms)

(With symptoms/some loss of vision)

(Permanent vision loss)
(Symptomatic/Non-symptomatic)

(Symptomatic)





(Permanent vision loss)
Pre-operative tests and instructions
A comprehensive dilated eye examination is the best way to diagnose diabetic retinopathy.
For this exam, dilating drops are placed in your eyes to widen your pupils to allow the doctor to have a better view of your eyes. The drops can cause blurred vision for a few hours till the effect wears off.
The other investigations used are:
1. Fundus Fluorescein Angiography (FFA)
After your eyes are dilated, a dye is injected into a vein in your arm. Pictures of the eye are taken as the dye circulates through your eyes’ blood vessels.
This helps us find the extent of damage to the retinal blood vessels, such as blocked vessels or broken or leaking blood vessels.
Fundus Fluorescein Angiography Machine
• Hi-tech digital imaging system
• Provides 25 photos of different eye angles in just 5 seconds
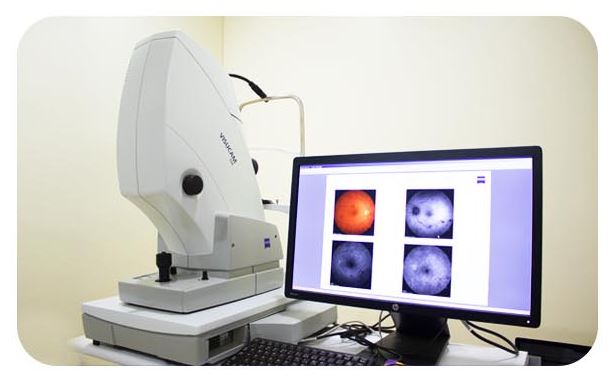
2. Optical Coherence Tomography (OCT)
This is a non-invasive test. Here, images of the retina are taken by the OCT machine after dilating the eyes. Sometimes, this test is possible without dilation too. The cross-sectional images show the thickness of the retina to determine how much fluid has leaked into the retina, causing swelling of the retinal layers.
OCT is used to determine the treatment modality. It is also used for post-operative examination to check the extent of reduction in swelling post-surgery or infection.
3. Blood Sugar Levels and HBA1C
Fasting and post-prandial (PP) blood sugar levels help know the control of blood sugars. HBA1C determines the 3-month average control of blood sugars.
A diabetes doctor or endocrinologist will help you to determine ways to improve your diabetes management if sugars are not under control, as this is important.
VEGF Inhibitors
If you have proliferative diabetic retinopathy or macular edema – swelling at the macula, you will need prompt treatment.
VEGF (Vascular Endothelial Growth Factor) inhibitors are medications which stop the growth of abnormal new blood vessels. They help reduce fluid leakage and build-up in the eye, and reduce swelling.
These are available in the form of injections, which are injected into the vitreous cavity of the eye under topical medication – anaesthesia drops like proparacaine.
These injections are repeated every month till the swelling reduces. In some cases, post-injection, laser photocoagulation is to be given to prevent further progression.
There are different Anti-VEGF medications such as;
• Bevacizumb – AVASTIN
• Ranibizumab – LUCENTIS
• Aflibercept – EYLEA
• Pagenex or Brolucizumab – PAGENEX
• Steroids – Triamcinolone and ozurdex
Side Effects
The injections are safe and effective but can cause mild, short
term discomfort which lasts around 24 hours;
• Burning sensation
• Formation of tears
• Build-up of eye pressure (in rare cases)
• Eye infection
Our doctors will monitor you during and after the treatment to
minimise the side effects.
Laser treatment is required when diabetic retinopathy is at proliferative stage, or there is diabetic maculopathy
(swelling in macula). Laser treatment is highly successful in halting the progress of the disease.
Process
After dilating the eye, the patient is taken to the laser room and made to sit in a comfortable position at the laser machine.
After giving anaesthetic, a hand-held lens is inserted into the eye.
An argon green laser beam is focused on abnormal blood vessels and microaneurysms in the retina which are highly
fragile and can easily cause bleeding into the eye.
The laser beam will seal the sources of leakage and repair damage
Focal Laser:
Small spots of laser 50-100 um are used and treated locally at abnormal sites with few laser spots.
Grid Laser:
Here, the macular area is treated when there is swelling or macular edema. The laser is shot in a grid pattern and focused on the macular area.
Pan-retinal photocoagulation (PRP):
This is commonly used in advanced cases of proliferative diabetic retinopathy. The whole of the retina is sealed with laser spots of 200-500 um. This is often combined with anti-VEGF injections to prevent the proliferation of new blood vessels and help stabilise the retina.
Eye surgery (Vitrectomy) – may be needed if:
• Large amount of blood has collected in your eye
• Extensive membranes are present which are likely to cause or have caused retinal detachment
• During the procedure, the surgeon will make a small incision in your eye before removing some of the vitreous humour,
removing any membrane and using a laser to prevent further deterioration in your vision
VEGF Inhibitors
If you have proliferative diabetic retinopathy or macular edema – swelling at the macula, you will need prompt treatment.
VEGF (Vascular Endothelial Growth Factor) inhibitors are medications which stop the growth of abnormal new blood vessels. They help reduce fluid leakage and build-up in the eye, and reduce swelling.
These are available in the form of injections, which are injected into the vitreous cavity of the eye under topical medication – anaesthesia drops like proparacaine.
These injections are repeated every month till the swelling reduces. In some cases, post-injection, laser photocoagulation is to be given to prevent further progression.
There are different Anti-VEGF medications such as;
• Bevacizumb – AVASTIN
• Ranibizumab – LUCENTIS
• Aflibercept – EYLEA
• Pagenex or Brolucizumab – PAGENEX
• Steroids – Triamcinolone and ozurdex
Side Effects
The injections are safe and effective but can cause mild, short
term discomfort which lasts around 24 hours;
• Burning sensation
• Formation of tears
• Build-up of eye pressure (in rare cases)
• Eye infection
Our doctors will monitor you during and after the treatment to
minimise the side effects.
Laser treatment is required when diabetic retinopathy is at proliferative stage, or there is diabetic maculopathy
(swelling in macula). Laser treatment is highly successful in halting the progress of the disease.
Process
After dilating the eye, the patient is taken to the laser room and made to sit in a comfortable position at the laser machine.
After giving anaesthetic, a hand-held lens is inserted into the eye.
An argon green laser beam is focused on abnormal blood vessels and microaneurysms in the retina which are highly
fragile and can easily cause bleeding into the eye.
The laser beam will seal the sources of leakage and repair damage
Focal Laser:
Small spots of laser 50-100 um are used and treated locally at abnormal sites with few laser spots.
Grid Laser:
Here, the macular area is treated when there is swelling or macular edema. The laser is shot in a grid pattern and focused on the macular area.
Pan-retinal photocoagulation (PRP):
This is commonly used in advanced cases of proliferative diabetic retinopathy. The whole of the retina is sealed with laser spots of 200-500 um. This is often combined with anti-VEGF injections to prevent the proliferation of new blood vessels and help stabilise the retina.
Eye surgery (Vitrectomy) – may be needed if:
• Large amount of blood has collected in your eye
• Extensive membranes are present which are likely to cause or have caused retinal detachment
• During the procedure, the surgeon will make a small incision in your eye before removing some of the vitreous humour,
removing any membrane and using a laser to prevent further deterioration in your vision
VEGF Inhibitors
If you have proliferative diabetic retinopathy or macular edema – swelling at the macula, you will need prompt treatment.
VEGF (Vascular Endothelial Growth Factor) inhibitors are medications which stop the growth of abnormal new blood vessels. They help reduce fluid leakage and build-up in the eye, and reduce swelling.
These are available in the form of injections, which are injected into the vitreous cavity of the eye under topical medication – anaesthesia drops like proparacaine.
These injections are repeated every month till the swelling reduces. In some cases, post-injection, laser photocoagulation is to be given to prevent further progression.
There are different Anti-VEGF medications such as;
• Bevacizumb – AVASTIN
• Ranibizumab – LUCENTIS
• Aflibercept – EYLEA
• Pagenex or Brolucizumab – PAGENEX
• Steroids – Triamcinolone and ozurdex
Side Effects
The injections are safe and effective but can cause mild, short
term discomfort which lasts around 24 hours;
• Burning sensation
• Formation of tears
• Build-up of eye pressure (in rare cases)
• Eye infection
Our doctors will monitor you during and after the treatment to
minimise the side effects.
Laser treatment is required when diabetic retinopathy is at proliferative stage, or there is diabetic maculopathy
(swelling in macula). Laser treatment is highly successful in halting the progress of the disease.
Process
After dilating the eye, the patient is taken to the laser room and made to sit in a comfortable position at the laser machine.
After giving anaesthetic, a hand-held lens is inserted into the eye.
An argon green laser beam is focused on abnormal blood vessels and microaneurysms in the retina which are highly
fragile and can easily cause bleeding into the eye.
The laser beam will seal the sources of leakage and repair damage
Focal Laser:
Small spots of laser 50-100 um are used and treated locally at abnormal sites with few laser spots.
Grid Laser:
Here, the macular area is treated when there is swelling or macular edema. The laser is shot in a grid pattern and focused on the macular area.
Pan-retinal photocoagulation (PRP):
This is commonly used in advanced cases of proliferative diabetic retinopathy. The whole of the retina is sealed with laser spots of 200-500 um. This is often combined with anti-VEGF injections to prevent the proliferation of new blood vessels and help stabilise the retina.
Eye surgery (Vitrectomy) – may be needed if:
• Large amount of blood has collected in your eye
• Extensive membranes are present which are likely to cause or have caused retinal detachment
• During the procedure, the surgeon will make a small incision in your eye before removing some of the vitreous humour,
removing any membrane and using a laser to prevent further deterioration in your vision
Anterior Segment Module: High-resolution OCT imaging for precise examination of the cornea, sclera, and anterior chamber angles, improving diagnostic accuracy.
Ultra-Widefield Angiography Module: Delivers evenly illuminated, undistorted, high-contrast scanning laser images for accurate retinal and vascular assessment.
OCT Angiography Module: Enables non-invasive vascular imaging, enhancing diagnostic capabilities without invasive procedures.
Simultaneous Fundus and OCT Imaging: Saves time and provides a comprehensive eye evaluation in a single examination.
TruTrack Active Eye Tracking: Ensures precise OCT imaging, even with patient movement, ensuring consistently reliable results.
Glaucoma Module: Offers a comprehensive analysis for early glaucoma diagnosis by matching scan patterns to relevant anatomical structures, aiding timely intervention.
High Standards of Power, Precision, and User Ergonomics: Ensures superb performance for effective treatments, resulting in better patient outcomes.
Excellent Ergonomics and True Portability: Offers convenient and mobile treatment solutions for healthcare professionals.
Quiet Operation: Eliminates distractions during treatment, ensuring a focused and peaceful environment.
Convenient, Easily Understood Controls: Facilitates a smooth interface with the laser system, enhancing treatment efficiency.
Full 2500 mW of Deliverable Laser Energy: Provides exceptional efficiency, leading to more effective treatments.
Variable Pulse Durations and Intervals: Customises treatment options with versatile settings for improved patient care.
It is an efficient and powerful surgical platform for vitrectomy surgery.
The device boasts great perfection, versatility, and innovative technology, as well as high user comfort with a compact design.
The Caliburn trocar system creates ideal access to the posterior segment and allows for smooth cuts and superb wound lightness.
The LED good light technology ensures excellent lighting conditions.
The pneumatic flow cutter benefits by allowing up to 10,000 cuts a minute and enables continuous flow and optimum positioning of vitreous body parts to be removed.
The innovative membrane FEELceps ensures strong and optimally dosed holding power and absolute precision.
Clear: IA
Poor blood sugar control and/or long-standing diabetes can cause changes in the blood vessels of the eye, causing diabetic retinopathy.
Controlling blood sugars is of utmost importance in stopping diabetic retinopathy from progressing. Also, a dilated eye examination every year, if you are a diabetic, helps diagnose the condition, and if it is treated well, progression can be halted.
Diabetic retinopathy does not give any symptoms in the early stage, but that does not mean that the disease has not progressed. In many cases, it is detected on the usual eye examination, where proper guidance and treatment can be given to halt the progression. Whether you have symptoms or not, it is better and mandatory to check your eyes once a year with a dilated eye examination.
Typically, diabetic patients can develop retinopathy at any stage, its very imp to have regular checkups through Ophthalmologists
Yes, if left untreated, diabetes leads to loss of vision, which cannot be restored.
With timely treatment, vision loss can be prevented, diabetic retinopathy progression can be delayed. After diabetic retinopathy treatment, you will have the best chance of a positive outcome if you manage your diabetes and keep your blood sugar well controlled.