- Academia
- For Corporate
- Cashless Facilities
- Media
- Donate
#NoCompromise
- 020 6609 9888 | +91 9168013322
#NoCompromise

To understand glaucoma, it is important to know what an optic nerve is. We have one optic nerve at the back of every eye – it comprises countless nerve fibres. It connects directly to your brain and sends visual messages to the brain to help you see.
Glaucoma is a disease of the optic nerve, in which the field of vision decreases gradually with time, leading to permanent blindness. Early detection and treatment are critical. But it requires regular monitoring and lifelong follow-up. The goal of the treatment is to preserve any existing vision and prevent further loss of vision.
Normally, glaucoma occurs due to a raised eye pressure.
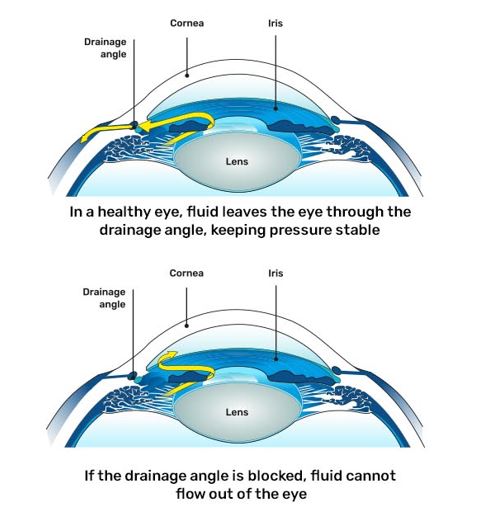
Our eyes constantly produce a clear fluid called aqueous humor which bathes and nourishes different regions of the eye. Typically, this fluid drains out of the eye through a drainage canal located at the angle of the eye. This angle is the junction between the cornea and the iris. In glaucoma, this fluid does not drain out as freely as it should. This increases the pressure inside the eye called Intraocular Pressure (IOP).
The normal intraocular pressure is between 10-22 mm of Hg. Raised IOP damages the optic disc, which is the part of the optic nerve seen within the eye. However, glaucoma can sometimes occur with a normal IOP – due to an extremely fragile nerve or reduced blood supply to the optic nerve. Hence, it takes more than measuring IOP to diagnose glaucoma.






The third type, developmental glaucoma, is further divided into:
Diagnosis of glaucoma requires a comprehensive eye examination and certain special investigations:
1. Slit lamp examination:
This special microscope is the ophthalmologist’s stethoscope, and all patients suspected of having glaucoma undergo a slit lamp evaluation.
2. Applanation tonometry:
The intraocular pressure is measured with an applanation tonometer attached to the slit lamp. This instrument is the gold standard for measuring the IOP. The non-contact tonometer uses an air puff to measure the IOP. It is good for screening but is not used for the diagnosis and treatment of glaucoma.
3. Gonioscopy:
In this test, after numbing the eye, a contact lens with a mirror is placed on the cornea to visualise the area from where the fluid inside the eye drains out. By this test, we come to know whether the angle is open or narrow or if there are any pigments or tears in the angle.
4. Ophthalmoscopy:
To diagnose glaucoma, we need to evaluate the optic nerve for signs of damage, and this is done by a dilated eye examination. A colour photo of the optic disc may also be taken for the documentation of optic disc damage and monitoring
1. Automated perimetry:
This is a test to map the field of vision. It detects the visual field damage caused by glaucoma. One eye is tested at a time, and you would be asked to look at a central fixation: dull yellow light and peripheral white lights of varying intensity are shown. When you see the peripheral white light, you need to press a small button in your hand. This is an important test to detect the functional loss of vision due to glaucoma.
Also, it is repeated at regular intervals to know whether your glaucoma is stable or progressing.
The drawback is that if you move your eye too much or are inattentive during the test, it can cause errors, and the test may have to be repeated. So you need to be as comfortable as possible during the test.
2. Pachymetry:
It detects the central corneal thickness. In this test, a small probe touches the central part of the cornea to measure the CCT. CCT influences intraocular pressure. Also, several studies have shown that those with a lower CCT have a greater risk of developing glaucoma and having progression as compared to those with a higher CCT.
3. OCT (Optical Coherence Tomography) Spectralis:
This scan compares the thickness of the optic nerve head and the surrounding tissue (RNFL) in different quadrants with that of a healthy individual of the same age and can detect glaucoma in the early stage.
4. Anterior Segment OCT(ASOCT):
This scan gives various measurements of the anterior chamber angle and can aid in the diagnosis of angle closure.
Timely treatment of glaucoma is necessary to
• Reduce eye pressure
• Halt the progression of the disease to permanent blindness
• Preserve the existing vision
Treatment is lifelong and requires regular follow-up. It depends on what type of glaucoma you have, and what treatments will work best for you. Your doctor will discuss the most suitable treatment for you after assessing your condition.
Surgeons can easily switch between posterior and anterior laser treatment – a space-saving and efficient solution
It focuses the optimum amount of laser energy onto the point of treatment, offering sensitive, high-precision treatment to patients using a minimum of laser energy
The fine gradations permit optimum regulation of the laser energy for the sensitive, minimally invasive treatment of your patients
The high-grade laser beam source is fully integrated into the laser slit lamp
The compact format of the flexible positionable control panel offers handy control of the user-friendly interface
The unique 4-point aiming beam ensures a high degree of aiming accuracy
The symmetrical arrangement of the control elements makes all slit lamp functions ergonomically accessible
A 180° tiltable tube is used as a viewing device for the surgeon, allowing them to work
Reduce visual field-testing time with NEW SITA™ Faster, improving patient satisfaction with perimetric testing and reducing patient fatigue
Reduces setup time with a single trial lens
SmartTouch interface on the HFA3 platform gets you up and running with fewer touches
Kinetic perimetry advancements provide an easy-to-use graphical user interface with a full 180° testing range
Improved confidence in test results with RelEYE™ - Instantly review the patient’s eye position, at any stimulus point
Unsurpassed in efficiency, the system is patient-responsive:
It learns to perform as fast as the patient wants to go
Excellent surgical outcome: Microscope image with optimum contrast and detail recognition along with a large depth of field
A 1:6 ratio zoom system allows the magnification of the overall system to be set as required by the surgical procedures.
A 180° tiltable tube is used as a viewing
As the incidence of glaucoma increases with age, it is mandatory after the age of 40 to have a complete eye examination. Risk factors include:
It can also be seen in newborns, which is called congenital glaucoma, or in children and young adults, called developmental glaucoma.